
Treatments & Surgery
Shock Wave Lithotripsy (ESWL) for Kidney Stones – Arlington & Dallas–Fort Worth
Non-invasive kidney stone treatment — no incisions, no scopes, no lasers.
When kidney stone pain hits, you want relief fast with the least invasive approach. That’s exactly what ESWL (Shock Wave Lithotripsy) delivers: focused sound waves from outside the body that break stones into passable pieces—often without a temporary stent and with minimal downtime. Dr. Richard Bevan-Thomas, board-certified urologist and founding partner of UPNT, offers high-volume ESWL in Arlington for quick scheduling at USMD Hospital Arlington (first floor) and at Surgical Centers of North Texas (outpatient).
Why Patients Choose ESWL with Dr. Bevan-Thomas
Our approach to Shock Wave Lithotripsy focuses on minimal invasiveness and rapid recovery:
- Truly Non-Invasive: No skin incisions, no scopes, no lasers.
- Outpatient & Quick Recovery: Most resume light activity in 1–2 days.
- Often No Stent: Many candidates avoid a ureteral stent (and its urgency/frequency).
- Effective for Many Stones: Ideal for stones typically ≤1.5 cm in the kidney or ureter.
- Targeted Imaging: Real-time X-ray or ultrasound for precise targeting of the kidney stone.
- All Options Available: If ESWL isn’t ideal, we offer ureteroscopy/laser (CULLS), PCNL, and a comprehensive stone prevention program for patients in the Dallas–Fort Worth, TX area.

How it Works
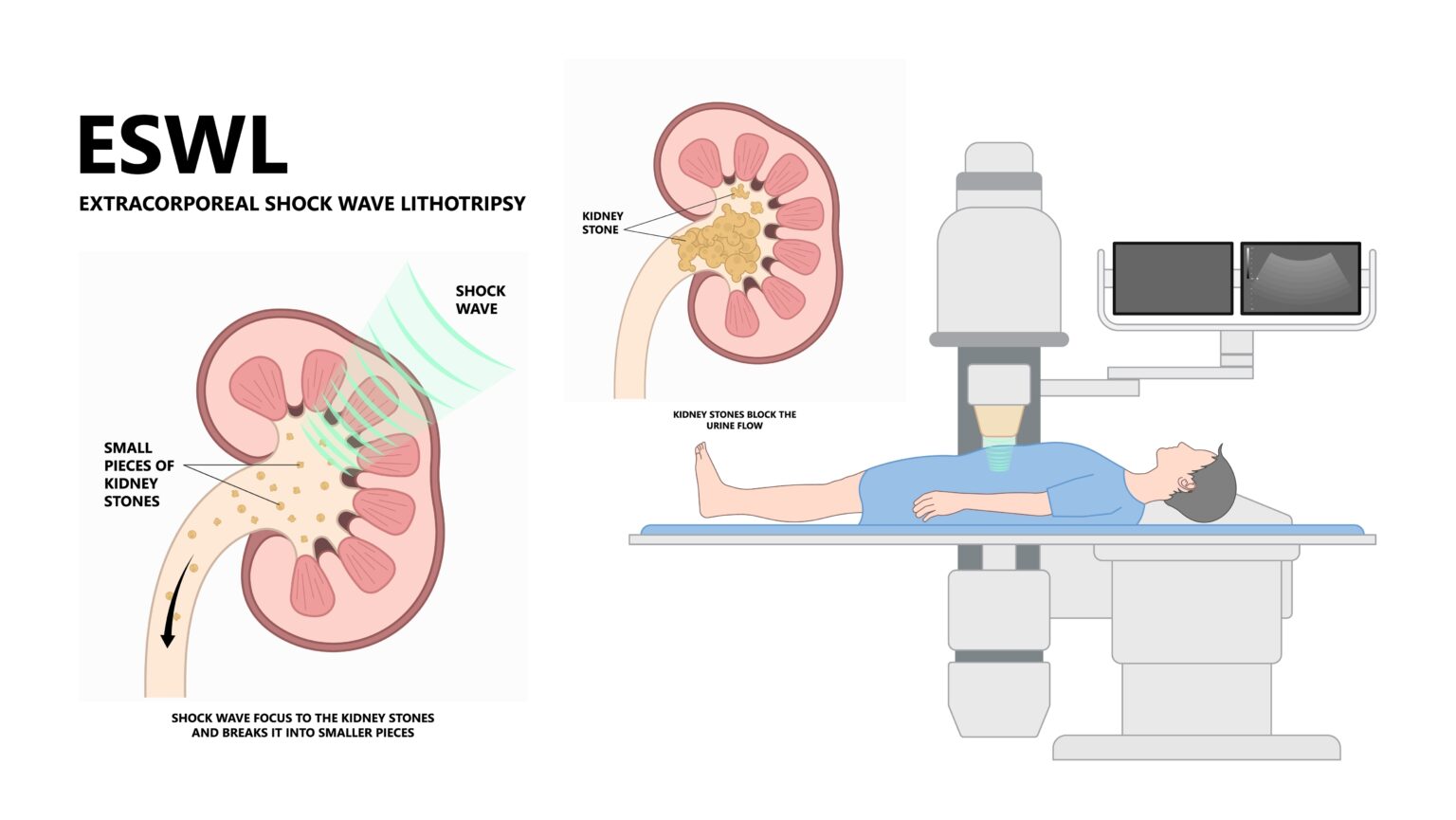
WHAT IS ESWL (Shock Wave Lithotripsy) & How it Works
ESWL uses a machine called a lithotripter to send thousands of focused shock waves through the skin. Soft tissues transmit the waves; the denser stone absorbs the energy and fractures into passable pieces.
- Targeting with X-ray and/or ultrasound.
- Comfort + Stillness under anesthesia.
- Precisely Aimed Pulses fragment the stone.
- Natural Passage over days to weeks.
For larger or lower-ureter stones, other options such as ureteroscopy (URS) or percutaneous nephrolithotomy (PCNL) may be more effective.
Am I a Candidate for ESWL?
In our program, most kidney stone patients are candidates, and for those patients, ESWL is typically first-line. You’re often a great fit if you have:
- Stones ≤1.5 cm.
- Stones in the kidney or any segment of the ureter (upper, mid, or lower).
- No pregnancy, no uncontrolled bleeding disorder, and no untreated infection.
We’ll review together:
- Stone density/hardness: Very hard stones may fragment less predictably.
- Body habitus / skin-to-stone distance: Deeper targets can reduce efficiency (we plan accordingly).
- Obstruction/Infection Risk: A temporary stent may be recommended for safety in select cases.
If ESWL (Shock Wave Lithotripsy) isn’t the best match, we’ll discuss ureteroscopy/laser (CULLS), PCNL, or short-term medical expulsive therapy when appropriate.
Benefits Patients Care About Most
- No incisions or scopes → lower infection risk, no scope-related urethral irritation.
- Outpatient → home the same day.
- Minimal downtime → light activity in 1–2 days; many back to work quickly.
- Often no stent → fewer urinary symptoms for many patients.
- Proven → excellent clearance in appropriately selected stones; repeatable if needed.
How Successful is ESWL?
Short answer: in appropriately selected patients, ESWL clears stones in the ∼80–90% range. Your personal outlook depends on stone size and density, location (kidney vs. ureter, lower-pole vs. other), and skin-to-stone distance—we walk through these together before treatment.
ESWL vs. Ureteroscopy (Laser) vs. PCNL — How We Decide
| Treatment | Indication / Key Benefit | Internal Link |
|---|---|---|
| ESWL | First-line for most eligible patients, especially stones ≤1.5 cm when a non-invasive, fast-recovery option is preferred; often avoids a stent. | |
| Ureteroscopy + Laser (CULLS) | Highest immediate clearance for many ureteral or high-density stones, or when ESWL isn’t ideal; usually includes a temporary stent. | Ureteroscopy (CULLS) |
| PCNL | For large/complex kidney stones (e.g., >2 cm, staghorn); tiny back incision in the OR. | PCNL for Large Stones |
Before, During, After ESWL
What to Expect
Before
- Urinalysis to rule out infection (treat first if positive).
- Medication review and safe management of blood thinners.
- Hydration unless contraindicated.
- Driver required due to anesthesia.
- Pre-anesthesia instructions for food/drink.
During (About 30 minutes)
- Anesthesia for comfort and stillness.
- Real-time targeting with X-ray/ultrasound.
- Focused shock waves fragment the stone.
After
- Same-day discharge.
- Hydration goal: keep urine light yellow/clear to help pass fragments (How to pass fragments faster).
- Pain plan: medications as needed; heating pad can help spasms.
- Strain urine if asked so we can analyze fragments (guides prevention).
- Activity: walk the same day; avoid heavy lifting for a few days.
- Follow-up & imaging to confirm clearance (ultrasound/X-ray as needed).
Prevention Matters
Future Stone Prevention
Dr. Bevan-Thomas personalizes a plan so you’re less likely to meet another stone.
- Stone analysis (composition).
- 24-hour urine testing (citrate, calcium, oxalate, uric acid, sodium, volume, pH) when indicated.
- Simple wins: Hydrate to 2–2.5 L urine/day; add citrate (lemons/citrus; Rx if needed); moderate sodium; maintain normal calcium with meals; oxalate awareness if advised; optimize weight/activity; adjust meds when appropriate.

Frequently Asked Questions
Is ESWL really the first treatment you recommend?
For most eligible patients, yes. It’s minimally invasive, outpatient, and has excellent results in appropriately selected stones.
Do you check for infection before ESWL?
Yes. We perform a urinalysis to rule out infection. If positive, we treat first and proceed once urine is clear.
Does ESWL hurt?
You’re under anesthesia during treatment. Afterward, discomfort is usually from passing fragments; we give you a pain plan.
Will I need a stent?
Often no. If there’s risk of blockage/infection, a temporary stent may be recommended for safety.
How soon will fragments pass?
Often within days, and passage can continue for several weeks. Hydration helps.
What if ESWL doesn’t clear everything?
We can repeat ESWL or use ureteroscopy/laser to clear the remainder—based on follow-up imaging and symptoms.
Is ESWL safe if I take blood thinners?
We’ll review your meds. Many blood thinners must be held safely before ESWL; we coordinate with your prescribing doctor.

About Dr. Rich Bevan-Thomas
- Robotic Surgery Volume: Over 3,000 robotic surgeries since 2002; refined catheter-free suprapubic recovery protocol.
- Technique: Meticulous nerve-sparing and endopelvic fascia-sparing techniques to support erections and early continence.
- Full Spectrum: Full-Spectrum Urologic Solutions: Offering advanced therapies, including Robotic Surgery (RALP), NanoKnife® (IRE) focal therapy, full-gland cryoablation, coordinated IMRT, and expert management for early-stage prostate cancer.
