
Prostate Inflammation in Arlington & Dallas–Fort Worth
Prostatitis (prostate inflammation) is a common condition that can be frustratingly chronic. Dr. Richard Bevan-Thomas provides accurate diagnosis and a structured management plan focused on long-term relief and symptom control for DFW patients. We aim to identify the cause quickly so you can begin conservative, effective treatment.

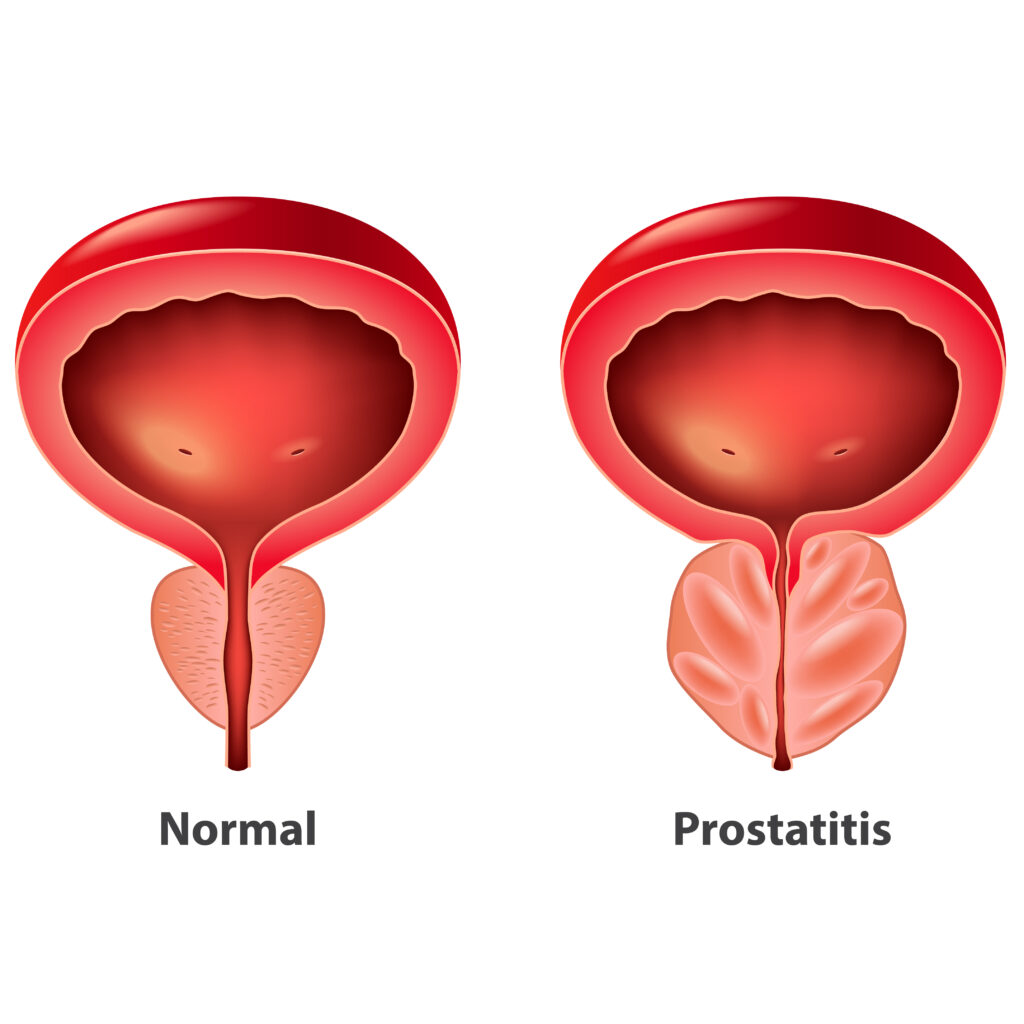
The Difference Between Inflammation, Enlargement, and Cancer
Prostatitis (inflammation) is often confused with Benign Prostatic Hyperplasia (BPH) (enlargement) or Prostate Cancer. As shown above, these are three distinct conditions:
Prostatitis: Involves inflammation and swelling, typically causing pain and urinary frequency, but it is not cancerous. It is often treated with antibiotics, lifestyle changes, or anti-inflammatories.
BPH (Enlargement): Involves non-cancerous growth, causing obstruction and urinary flow issues, but usually not pain.
Prostate Cancer: Often presents with no symptoms at all and is found through screening (PSA/biopsy).
Dr. Bevan-Thomas specializes in accurate diagnosis to ensure your symptoms are properly identified, ruling out serious conditions like cancer early in the process.
Understanding Prostatitis
Prostatitis—inflammation of the prostate—is one of the most common and misunderstood urologic conditions in men. It can cause groin/pelvic pain, burning with urination, and difficulty emptying the bladder. Some men have mild, episodic discomfort; others develop severe symptoms that disrupt work, sleep, and intimacy.
Nearly half of all men experience prostatitis symptoms at some point. My goal is to make the cause clear and design a step-by-step plan that relieves pain and prevents future flare-ups.
What Causes Prostate Inflammation?
Prostatitis isn’t one single disease. The right treatment depends on the type:
Bacterial Prostatitis
Bacteria from the urinary tract (often E. coli, Klebsiella, Proteus) can infect the prostate.
Typical symptoms
- Burning or pain with urination
- Fever or chills
- Weak/interrupted urine stream
- Pelvic or lower back pain
Accurate testing matters: Standard urine cultures can miss infections. When needed, I use DNA-based RT-PCR urine testing to improve detection.
Non-Bacterial (Chronic) Prostatitis / CPPS
Inflammation without active infection. Common drivers:
- Prolonged sitting (driving, cycling, desk work)
- Dehydration
- Pelvic floor muscle tension
- Autoimmune response or prior infections
Think of the prostate like a sponge—hydrated = relaxed/open; dehydrated = tight/irritable. Alcohol and caffeine can worsen symptoms; water, movement, and relaxation help.
Common Symptoms of Prostatitis
What Causes Prostate Inflammation?
- Dull ache/pressure in the perineum, groin, lower back, or scrotum
- Burning or pain during urination
- Urgency/frequency; nocturia
- Pain with ejaculation
- Weak stream or incomplete emptying
- Occasionally decreased libido or erectile discomfort (secondary to pain)
Urgent warning: If you develop fever, chills, or inability to urinate, seek immediate medical care—this may indicate acute bacterial infection requiring antibiotics and, at times, temporary bladder drainage.

Diagnosis
How We Diagnose Prostatitis
A precise diagnosis prevents unnecessary antibiotics and targets the real cause.
Your evaluation may include:
- Urinalysis & culture (with PCR testing when appropriate)
- Prostate exam to assess tenderness or swelling
- Bloodwork (CBC, CRP) if infection suspected
- PSA (delayed until symptoms improve to avoid false elevation)
These scans guide us toward the most effective therapy—whether the cancer is confined or more advanced.
Treatment Options for Prostatitis
Antibiotics (If Bacteria Are Found)
- Typical course 2–6 weeks (longer in chronic cases)
- Preferred options: Bactrim or Ceftin guided by sensitivities
- I avoid routine fluoroquinolones (Cipro/Levaquin) due to resistance and tendon risks
Alpha Blockers
- Alfuzosin (Uroxatral) or Tamsulosin (Flomax) relax the bladder neck/prostate to improve flow and reduce pressure
- I often favor Alfuzosin for its lower sexual side-effect profile
Anti-Inflammatory Therapy
- NSAIDs: ibuprofen, naproxen, or Celebrex profile
- For severe flares: short Medrol Dosepak to interrupt the pain–inflammation cycle

Dr. Bevan-Thomas’ Prostatitis Recovery Plan

DR. BEVAN-THOMAS’ PROSTATITIS RECOVERY PLAN: 5 Steps to Symptom Control
- Hydration Aim for 2–3 liters/day (water or sugar-free electrolytes). Limit energy drinks, sodas, and excess caffeine.
- Cranberry Extract (GennaMD) Contains 36 mg soluble PAC to help prevent bacterial adherence; take 1 capsule daily.
- Epsom Salt Baths – 2 cups in warm water for 20 minutes nightly to relax pelvic muscles and improve blood flow.
- Move Daily – Walking, swimming, or cycling with breaks improves pelvic circulation and reduces flares.
- Stress Management Stress tightens the pelvic floor. Try 10 minutes/day of guided breathing or Headspace meditation.
When to Seek Medical Care
- Stay well-hydrated
- Limit alcohol and caffeine
- Avoid long periods on hard seating; take standing/walking breaks
- Eat a produce-rich, anti-inflammatory diet
- Exercise regularly and manage stress

Frequently Asked Questions
Is prostatitis the same as prostate cancer?
No. Prostatitis is inflammation or infection; prostate cancer is uncontrolled growth. Symptoms can overlap, but prostatitis does not raise cancer risk.
How do I know if my prostatitis is bacterial or not?
Bacterial cases often have fever/chills and acute pain. Non-bacterial tends to be chronic pelvic discomfort without infection. Urine culture or PCR testing clarifies the type.
How long does prostatitis take to resolve?
Acute cases often improve in 2–6 weeks with antibiotics and hydration. Chronic cases may take months—hydration, pelvic relaxation, and anti-inflammatories are key.
What makes prostatitis worse?
Dehydration, alcohol, caffeine, prolonged sitting, and stress. Counter with hydration, movement, warm baths, and anti-inflammatories as directed.
What should I do if I develop a fever or can’t urinate?
Go to the emergency room now. You may need antibiotics and/or temporary catheter drainage to protect the bladder and kidneys.
Schedule Your Consultation
If conservative management has failed, schedule a specialist evaluation with Dr. Bevan-Thomas. We focus on accurate diagnosis (including advanced DNA testing) to design a clear, long-term plan for chronic or recurrent symptoms—right here in Arlington and DFW.
- 866-367-8768
- 801 West I-20 Suite 1 • Arlington TX 76017
